Another look at androgen receptor gene variants in trans women →
Note: Some images depict small amounts of blood.

Hair is an item of significant concern for trans people during transition: hair, its style, and its presence or absence in various areas can be a factor both in one’s experience of gender dysphoria as well as how one’s gender is seen and attributed by others. The most widely known form of hair management is laser hair removal or electrolysis used by trans women and transfeminine people for the permanent removal of unwanted facial and body hair, including from the genitals prior to vaginoplasty. Trans women may also experience male-pattern baldness from years of prior testosterone exposure, making use of treatments such as minoxidil to stimulate scalp hair regrowth (although a degree of scalp hair regrowth has sometimes been reported as a result of HRT alone).
However, a much wider variety of possibilities for hair restoration, alteration, and management – including many I’d never heard of until now – are available for both trans women and trans men through surgical means. Bared & Epstein (2019) provide an enlightening summary of these techniques and the results that can be achieved.
Hairline lowering via scalp advancement is a commonplace part of facial feminization surgery (Garcia-Rodriguez, Thain, & Spiegel, 2019), but this can also be achieved by transplantation of hair to the hairline from other sites, and the authors detail the specific parameters that are sought when feminizing the hairline via hair transplantation:
A soft, heart-shaped hairline design with rounded recession in the frontal-temporal region is often used to feminize the hairline and achieve a natural appearance to the hairline. To aid in the creation of a natural hairline appearance, often a subtle widow’s peak is created slightly off-center. Rounding of the hairline is then performed posteriorly and laterally along the frontal-temporal region, connecting to the temporal points.
Using hair transplantation, a full beard can be created to a specified design, potentially including the sideburn, cheek, mouth, goatee, and mustache areas:

The authors state that in their experience, “the scalp hair transplants to the face have a high regrowth percentage and, if properly performed, patients can achieve a natural outcome” and that “patients are always made aware of the possibility of undergoing secondary procedures after approximately 1 year if further density is desired.”
Hair transplantation can also be used to create and reshape eyebrows into a typically or masculine shape:
The masculine eyebrow shape is generally less arched but comes to a lateral widening at the peak of the brow, whereas the feminine eyebrow shape is more rounded and arched.

Additionally, large-scale hair grafting (“procedures of 1800 grafts to as many as 3000 grafts are indicated”) can be used in trans men to create chest hair, which can also serve to cover up scars from chest reconstruction surgery:
These potential areas, depending on patient goals, can include the upper and central chest, ranging laterally and inferiorly (particularly to conceal mastectomy scars) and even continuing caudally in a vertical direction into the abdomen and even upper pubic region. The keys to achieving a natural result, besides careful acute angulation of the recipient sites, is to have a crossed-hatch pattern of hair growth toward the midline, that is, the sternum.

Such procedures could be particularly beneficial to trans men given previous findings that even with testosterone, not all trans men will develop as much chest hair as cis men. This review helps to affirm that medical progress for trans people is still happening, and new methods are always being developed for the improvement of body image and the effective treatment of bodily gender dysphoria. ■

About Zinnia Jones
My work focuses on insights to be found across transgender sociology, public health, psychiatry, history of medicine, cognitive science, the social processes of science, transgender feminism, and human rights, taking an analytic approach that intersects these many perspectives and is guided by the lived experiences of transgender people. I live in Orlando with my family, and work mainly in technical writing.
View all posts by Zinnia Jones →
This entry was posted in Dermatology, Surgery and tagged medicine, transition. Bookmark the permalink.

Gender identity, including in trans people, appears to have a physical basis and a biological underpinning, and the Endocrine Society has stated that numerous features suggest trans people’s genders are a matter of likely prenatal development:
Such evidence stems from scientific studies suggesting that: 1) attempts to change gender identity in intersex patients to match external genitalia or chromosomes are typically unsuccessful; 2) identical twins (who share the exact same genetic background) are more likely to both experience transgender identity as compared to fraternal (non-identical) twins; 3) among individuals with female chromosomes (XX), rates of male gender identity are higher for those exposed to higher levels of androgens in utero relative to those without such exposure, and male (XY)-chromosome individuals with complete androgen insensitivity syndrome typically have female gender identity; and 4) there are associations of certain brain scan or staining patterns with gender identity rather than external genitalia or chromosomes.
The developmental origin of gender identity has led researchers to look for distinct genetic features that may play a role in the development of a gender identity contrary to assigned sex. One area of focus is genes related to sex hormones, as differences in the functioning of sex hormones may affect the degree of prenatal masculinization of the brain, potentially altering gender identity even as the rest of the body develops normally (Foreman et al., 2019). Hare et al. (2009) reported the promising result that among 112 trans women, a greater number of repeats of the CAG sequence were present in the androgen receptor (AR) gene compared to cisgender men. The authors note that this longer length results in androgens such as testosterone being less effective at activating the androgen receptor, possibly resulting in reduced brain masculinization prenatally.
However, despite the differences in prevalence between trans women and cis men in the study, there was a great deal of overlap: 44.6% of the studied trans women did not have the “long” AR variant potentially causing reduced androgen signaling, while 47.6% of the cis men did have this variant. Additionally, a later study (Ujike et al., 2009) did not replicate this result, finding no significant differences in CAG repeats in the AR between trans women and cis men:
So: Do trans women tend to have a variant of the AR gene that reduces androgen signaling, or do they not? A recent meta-analysis seeks to resolve this uncertainty.
D’Andrea et al. (2020) posit that “small sample sizes in most studies might have contributed to inconclusive results”, and proceed to perform a systematic review of five studies that included information on CAG repeats in trans women’s AR genes. Examining data from a total of 795 trans women and 1,355 cis men, the authors found that “the length of CAG repeat sequences of AR gene was significantly longer in the trans woman group” (p = 0.005). Nevertheless, as with Hare et al., this variant alone is not a reliable indicator of transness:
…the gene polymorphism investigated in the present study is relatively common, suggesting that the revealed association would not reflect a direct independent causal link. It is likely, indeed, that variants in different sex hormone signaling genes involved in brain sexual differentiation, together with other factors, could influence the development of gender identity/incongruence.
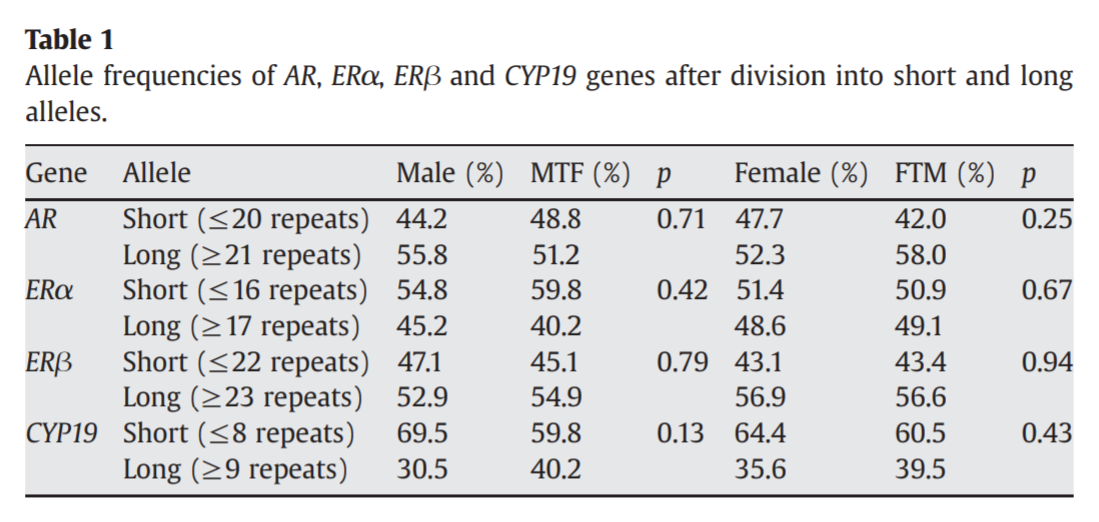
In other words: this is not some kind of “trans gene” that can be used to distinguish a trans woman from a cis man just by looking at this one sequence. Instead, the developmental aspects of gender identity may be influenced by many genes related to sex hormones, or interactions between combinations of these genes. Foreman et al. (2019) did not find a difference in AR CAG repeats between trans women and cis men, but four combinations of gene variants were found to be overrepresented in trans women compared to cis men, and three of those combinations involved the long repeat length variant of the AR. The study also identified a number of other gene variants that could alter the functioning of sex hormones in trans women:
Although long CAG repeats in AR alone may not have an independent effect on the development of gender dysphoria, this AR polymorphism may interact with other genes to increase the likelihood of being transgender. … Similarly, long repeats in ERβ have been associated with decreased ERβ signaling, potentially reducing the influence of ERβ on the defeminization of the male brain. In combination, both genotypes appear to have additive effects on the development of gender dysphoria. … Interaction analysis also identified the specific combination of SRD5A2 and CYP17 polymorphism, the former associated with reduced levels of DHT, whereas the latter is known to increase sex steroid precursor production. It seems plausible that together, these polymorphisms may increase the production of precursor steroids and testosterone, but not of DHT, the more potent androgen form.
The authors are careful to highlight that “although discordance rates for gender dysphoria suggest that genetics plays a role, it is not the sole determinant of gender identity.” Additionally, there is the possibility that genetic studies utilizing much larger sample sizes may reveal that these findings of overrepresented gene variants in trans women were false positives – and it may be difficult to acquire genome data from the much larger number of trans women required to offer reasonable assurance that these results are not spurious. Nonetheless, if these are indeed true positive findings, they may provide a valuable piece of the puzzle on the nature, origin, and development of gender dysphoria. ■

About Zinnia Jones
My work focuses on insights to be found across transgender sociology, public health, psychiatry, history of medicine, cognitive science, the social processes of science, transgender feminism, and human rights, taking an analytic approach that intersects these many perspectives and is guided by the lived experiences of transgender people. I live in Orlando with my family, and work mainly in technical writing.
View all posts by Zinnia Jones →
This entry was posted in Endocrinology, Gender dysphoria, Genetics and tagged science. Bookmark the permalink.
Disclaimer: I am not a medical professional and this is not medical advice.

While trans women on HRT typically require testosterone blockers in addition to estrogen to reduce testosterone to the desired levels and produce effective feminization, trans men generally require only testosterone to achieve physical masculinization. However, one potential concern is the effect of aromatase, an enzyme which can convert testosterone into estrogen. Testosterone treatment in cis men has been associated with high estrogen levels in 20% of men in one study (Tan, Cook, & Reilly, 2015), and can produce physical effects such as gynecomastia (Rhoden & Morgentaler, 2004).
Testosterone treatment for trans men aims to induce testosterone levels within the typical male range (Hembree et al., 2017), while levels of estrogen are not usually as much of a concern, although clinicians have raised the possibilities that testosterone treatment could cause either unwanted high estrogen levels through aromatization or unhealthily low estrogen levels through suppression of estrogen production. A recent study of 746 trans men and transmasculine people taking testosterone seeks to answer these questions, measuring the effects of testosterone on their estrogen levels.
Defreyne et al. (2020) recorded trans men’s estradiol blood levels at baseline before starting testosterone, as well as after 3, 6, 9, 12, 18, 24, and 36 months of testosterone. The authors found that estradiol levels decreased by an average of 17.1 pg/mL over the first three months of treatment, and there was also a statistically significant decrease of an average of 19.6 pg/mL between months 12 and 18. Additionally, over a 1-year followup, use of longer-acting injectable testosterone undecaonate was associated with lower estradiol levels than use of other shorter-acting injectable testosterone esters or testosterone gel, with the authors noting that testosterone undecaonate “is less susceptible to fluctuations in serum testosterone levels and may provide a more sustained gonadotropin and menstrual cycle suppression and may result in less aromatization to estradiol”
Interestingly, by 36 months, trans men who had undergone hystero-oophorectomy (which includes removal of the ovaries) had estradiol levels similar to those who still had ovaries. However, overall, the trans men in the study still had estradiol levels higher than those typical of cis men even after testosterone treatment. The authors conclude that testosterone does not appear to produce higher estradiol levels or physical effects in trans men: “it is unlikely that testosterone therapy in AFAB people could be a risk factor for undesired estrogenic effects, including persistent menstrual cycle, pelvic pain, and gynecomastia.” Testosterone produced “suppression of endogenous estradiol production”, and moreover, “the observed decrease in serum estradiol levels does not lead to adverse outcomes, unlike in hypogonadal females.” They further state that aromatase inhibitors, which block testosterone from being converted into estrogen, should not be used due to the potential harm of unhealthily low estrogen levels:
Lower estrogen levels at menopause lead to accelerated bone loss. Therefore, aromatase inhibitors should not be used in the masculinizing hormone regimen due to potential bone loss.
These findings confirm the results of another study of 34 trans men treated with testosterone over the course of six years (Chan et al., 2018). In this study, testosterone was given as short-acting testosterone enanthate or testosterone cypionate, typically injected weekly. Estradiol levels were observed to decrease from an average of 81 pg/mL at baseline to a steady average of 54 pg/mL during treatment. The authors note that “it is extremely unlikely that there was an unappreciated rise in serum estradiol levels secondary to aromatization from exogenous testosterone”, and that “the decrease in serum estradiol levels provides some support for more recent proposals that there is no extra risk to female reproductive tissues, such as endometrium, cervix, and breast tissue, from androgen exposure at normal male levels.” They likewise conclude that there does not appear to be a need for the use of aromatase inhibitors to decrease estradiol levels.
Altogether, it appears that trans men using testosterone do not need to be concerned about the possibility of increased estradiol levels or reproductive cancers resulting from estrogenic effects, and do not require any additional medication to suppress estradiol. ■

About Zinnia Jones
My work focuses on insights to be found across transgender sociology, public health, psychiatry, history of medicine, cognitive science, the social processes of science, transgender feminism, and human rights, taking an analytic approach that intersects these many perspectives and is guided by the lived experiences of transgender people. I live in Orlando with my family, and work mainly in technical writing.
View all posts by Zinnia Jones →
This entry was posted in Endocrinology, Transmasculine and tagged HRT, transition. Bookmark the permalink.




































